
Highlighting compassionate, evidence-based paths to recovery
By Hilary Disch
This National Recovery Month, we are highlighting PPP’s Medication for Opioid Use Disorder (MOUD) clinic, and particularly the medication Sublocade, which has proven immensely successful for many of our patients experiencing opioid use disorder (OUD). Read on to find out about the clinic, MOUD (known as the “gold standard” of treatment by medical professionals around the country), and how Sublocade is helping so many people reach their self-defined recovery goals.
A Low-barrier Clinic in the Heart of Kensington
"We’re working with a population that is pretty consistently living unsheltered and injecting fentanyl,” says Chad Gurdgiel, coordinator of STEP at PPP. “We provide all the different buprenorphine products like oral Suboxone and injectable Sublocade. We also have the capability to do Vivitrol.”

Chad and his colleague Brad Meck, a clinic case manager, emphasize that the PPP clinic is extremely low barrier. Each participant is paired with a case manager who offers wraparound social services, but there are very few requirements beyond that.
“All we ask is that you show up, you take the medication, you meet with us,” Chad clarifies. Unlike many other clinics, PPP does not turn participants away if they continue to use fentanyl.
Challenges to Medication-Assisted Recovery: Stigma, Diversion, and Induction
Unfortunately, there is still a lot of stigma around MOUD, particularly in traditional recovery settings.
"Some 12-Step groups assume that you’re not technically ‘clean’ if you’re on meds,” says Brad, who has been in recovery from OUD for 10 years thanks to Suboxone. “I don’t really care about that... buprenorphine saves lives and increases patients’ quality of life by an immeasurable amount.”
"The fact of the matter is that buprenorphine is safer than Tylenol, and some people need to be on it forever, and that is totally fine."
Chad agrees. “A lot of what we see is folks coming into our program that internalize a lot of that stigma. Even in the induction phase, they might say that their ultimate goal is to be off everything, that this is only a temporary solution because ultimately ‘sobriety’ is what they must work towards."
Chad’s team dispels myths about MOUD and reassures participants that using medication is a valid form of recovery.
“The fact of the matter is that buprenorphine is safer than Tylenol, and some people need to be on it forever, and that is totally fine,” Chad emphasizes.
A decade into his recovery, Brad is still on Suboxone. “I got on, and was free of withdrawal. I'd spent 10 years of my life in withdrawal every day. I thought, I never want to feel that again. I’m a normal human being for God’s sake. It's beautiful.”
Another unique challenge faced by PPP participants is that there is a large street demand for buprenorphine in Kensington. According to the STEP team, when a participant leaves the pharmacy, they are often met by people offering cash for their buprenorphine. This constant temptation is perhaps the biggest challenge to induction, which is, in itself, extremely difficult for most people with OUD.
“Buprenorphine has such a high affinity for the opioid receptors that if you introduce it while there is still fentanyl on the receptors, it will put you into precipitated withdrawal — your standard withdrawal symptoms times a hundred,” Chad says.
"We’re so much more intentional about induction."
The psychoactive effects of fentanyl have a short half-life, but it is fat soluble so it stays in the body for much longer than heroin or oxycodone. If a participant has a fentanyl addiction, it can take 48 to 72 hours of waiting before buprenorphine can be introduced. That wait, Brad states, is brutal.
“Movies don’t even get it correctly. [Withdrawal] is horrific.”
Because of severe withdrawal, the PPP’s clinic has adjusted its induction process to fit the needs of our demographic. Providers start patients on buprenorphine with a micro-induction, recognizing that most participants are not going to stop using fentanyl right away.
“We start them really low, sometimes with a half of one milligram during the first days,” Brad explains.
The team then introduces more buprenorphine over the course of a few days, while the participant slowly decreases their fentanyl intake, what Chad refers to as a “gentle transition of titrating up and titrating down.”
"Most other clinics don’t have time or don’t pay attention to induction... We’re so much more intentional about induction. We want to know: What are you going to do when you walk out of here? How much are you taking? Let’s only give you that amount so you’re not walking around the street with the temptation to sell it all,” Chad says.
What is Sublocade?
In addition to the clinic’s individualized induction process, the injectable medication Sublocade has been a game-changer in navigating obstacles to medication adherence. While Suboxone has a diversion risk for its street value, Sublocade is injected into the patient’s stomach one every four weeks.
“You don’t have to remember to take it anymore. It’s just inside you and it slowly provides buprenorphine in your blood stream,” Brad explains.
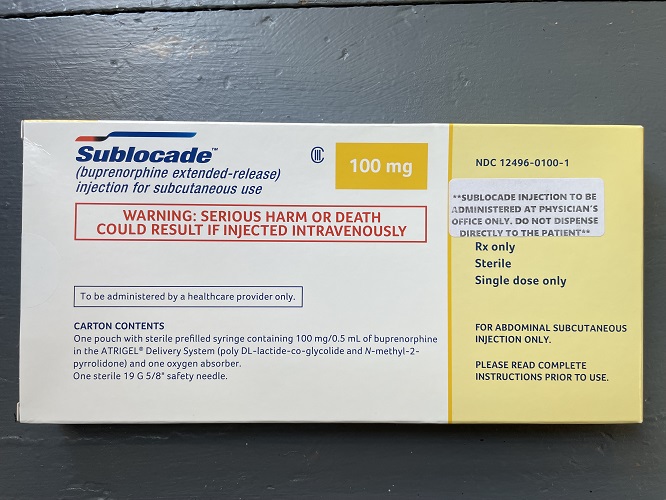
According to Chad, it is standard practice at other clinics to start a patient on a “loading dose” of 300 milligrams and then quickly go down to a maintenance dose of 100 milligrams until the doctor takes the patient off the medication completely.
However, as with any of the other medications, STEP tailors treatment with Sublocade to the individual.
"We do a 300-milligram loading dose and we’ll do that as long as the patient wants because we know our patients are using fentanyl,” Chad explains. “A lot of our folks have really high tolerance and need more buprenorphine for a longer period of time.”
Every month, between 15 and 20 people are receiving Sublocade injections at the clinic. Chad says that incentivizing participants for their injections is correlated with higher success rates.
“The theory always was, what does somebody make in a month on the street from selling their medication? Can we pay somebody that much to get a Sublocade injection? We're doing it now. We're giving everyone $100 in Visa gift cards every time they get their injection,” he says.
Success with Sublocade
Joey Scalia, a PPP participant for the past seven years, developed OUD in 2016. He says that he had been to rehab at least six times before finally connecting with his case manager Brad Meck and beginning Sublocade. Today he is proud to say he has not used fentanyl in eight months.
“When I left rehab before, I would relapse and relapse and relapse,” Joey recalls. He found out about Prevention Point’s MOUD clinic from word-of-mouth on the street. He first tried Suboxone, but it was not a successful match for him, as he had trouble keeping track of the medication and managing a daily dose.
“I got [Sublocade] about seven months ago and it works fine. You don’t have to keep track of it, you know what I mean? You just have to renew the injection monthly with the doctor,” Joey says.
The combination of Sublocade along with frequent check-ins with Brad and the doctor have been exactly what Joey needs to meet his recovery goals.
“I come here every day if I’m not working. It’s like a safe haven. They’re nice to everybody I’ve known. I actually only come here,” Joey emphasizes.
“Sublocade is like a miracle drug. It doesn’t interfere with eating or sleeping, it doesn’t make you high. I’ve told so many people about it.”
